Vitamin B12 Deficiency Anemia
One of the severest consequences of having a short supply of B12 is vitamin B12 deficiency anemia. This refers to an extreme form of anemia, which can be deadly if untreated (1-3).
Vitamin B12 together with folic acid plays an important role in cell division and DNA synthesis. Vitamin B12 deficiency therefore extremely impairs not only the regeneration of the vessels and organs, but also the new formation of blood.
Since a steady supply of vitamin B12 has numerous benefits and is essential to good health; a long-term vitamin B12 deficiency can lead to a dangerous form of anemia, which can have grave consequences for health.
The Symptoms of Vitamin B12 Deficiency Anemia
The typical symptoms of vitamin B12 anemia include:
- Chronic fatigue
- Impaired physical performance
- Pale skin
- Increased heart beat
- Collapse
- Inflamed, smooth tongue (atrophic or hunter glossitis)
- Digestive disorders
- Chronic gastritis type A (autoimmune gastritis)
Further Symptoms of Vitamin B12 Deficiency
As a result of B12 deficiency – often before anemia has even been detected – various nerve disorders (neuropathies) occur. These are characterised by mild to severe discomforts, such as: numbness of the skin, hands and/or feet; tingling sensations; unsteadiness in walking and coordination disorders – but can also develop into severe paralyses and pains.
If left untreated, irreversible damage to the nerves and spinal cord can occur, since the myelin nerve-protection layer is attacked. Without this protective layer, the nerves can be destroyed, leading to various clinical pictures such as spinal cord degeneration (funicular myelosis) (4, 5).
More information: Vitamin B12 and Nerves
At the same time the synthesis of hormones and neurotransmitters is disturbed, meaning that often psychological symptoms accompany physical ones, such as: concentration difficulties, poor memory, depression, psychosis, schizophrenia and dementia (6).
See here: Vitamin B12, Brain and Psyche
Diagnosis and Appearance of Vitamin B12 Deficiency Anemia
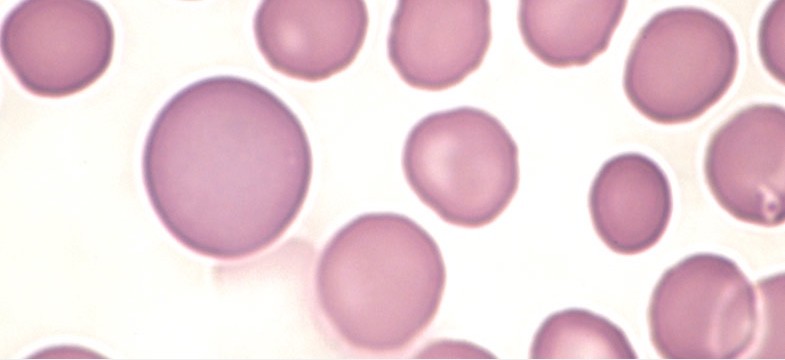
Vitamin B12 anemia is a type of so-called megaloblastic anemia. It is characterised by an increase in red blood cells (erythrocytes) and an increased haemoglobin content.
Disturbed DNA synthesis leads to a maturation disorder of the erythrocytes, which get trapped at an early stage of development. In the blood, this is demonstrated by greatly enlarged red blood cells, known as megalocytes, and in the bone marrow by megaloblasts – hence the term “megaloblastic” anemia. Megalocytes and megaloblasts each originate from immature progenitor cells of the red blood cells (7).
In the blood count, the values of the MCV (mean corpuscular volume) and MCH (mean corpuscular haemoglobin) are normally significantly increased, while the vitamin B12 level is strongly decreased.
Under the microscope, hypersegmented, aged neutrophils also appear; a subgroup of white blood cells.
However, as we will see below, it is not always possible to make a diagnosis based on the blood count, due to the poor accuracy of B12 serum tests. Plus, other nutrient deficiencies can alter results, masking B12 deficiency.
Causes of Vitamin B12 Deficiency Anemia
Vitamin B12 anemia is triggered by B12 deficiency, which can have various causes (8). The most common include:
Malabsorption
- Pernicious anemia (see next paragraph)
- Bowel resections
- Gastritis and other intestinal diseases
- Helicobacter pylori infection
- Tapeworms
- Zollinger-Ellison syndrome (increased gastrin production)
More information: Vitamin B12 Malabsorption
Deficient supply
- Poor diet
- Vegan and vegetarian diets
- Increased requirement due to pregnancy and lactation or stress
Interactions
- Nitrous oxide/laughing gas
- Alcohol and drugs
- Medicines (anti-epileptic drugs, antibiotics, acid blockers, etc.)
Pernicious Anemia
The term pernicious anemia is often used interchangeably with vitamin B12 deficiency anemia. Strictly speaking, however, the former refers only to cases of B12 anemia triggered by a lack of intrinsic factor (7).
Intrinsic factor (IF) is a special transport protein that is responsible for the intake of vitamin B12 from food and is produced by the parietal cells in the stomach. Pernicious anemia is a consequence of type A gastritis. Due to this chronic inflammation of the gastric mucosa, the immune system triggers the production of antibodies that fight the parietal cells and IF. As a result of the subsequent IF deficiency, no further B12 can be absorbed, which can lead to the above-described megoblastic anemia (9-11).
Pernicious anemia can be distinguished from other forms of B12 deficiency anemia by various tests, although gaining absolute proof is difficult.
Antibodies against the IF and the parietal cells can now be detected through special tests, with a current accuracy of only 30-70% (12, 13).
The diagnosis is also made through the detection of gastric mucosa atrophy with simultaneous gastric acid deficiency.
The unambiguous Schilling test, which used to be carried out for diagnosis, is no longer offered today due to its expense.
Treatment of Vitamin B12 Deficiency Anemia and Pernicious Anemia
B12 anemia therapy consists primarily of eliminating the vitamin deficiency. Depending on the cause, however, the therapy may also include further steps.
As with all forms of B12 deficiency, therapy proceeds in two phases (14):
- High dose initial therapy
To quickly eliminate the deficiency and replenish the body stores - Maintenance therapy
Maintaining blood levels with a maintenance dose
In the case of pernicious anemia, maintenance therapy must be continued for life due to the IF antibodies, since there is currently no remedy for the causes of this autoimmune reaction (15).
The situation is different in the case of a poor diet or other intake disorders, such as bacterial or parasitic infections, since the causes can be addressed and normal B12 absorption restored.
Injections or Oral Supplements?
For a long time, B12 injections were regarded as the only vitamin B12 supplement viable for treating pernicious anemia, since vitamin B12 absorption via IF is not possible here.
Today, however, we now know that there is also a passive intake route for vitamin B12: about one percent of each dose taken reaches the intestinal wall and blood via passive diffusion. With an adequately high dosage, oral supplements are able to treat all forms of B12 deficiency, as numerous case reports and studies confirm (16–18).
For the treatment of anemia, at least 1000 µg of vitamin B12 per day are recommended to be taken orally. However, a faster recovery can be achieved with doses between 5000 – 15 000 µg.
Comparison of Intakes
Common Dose (µg) | Average Intake (µg) | |
Cyanocobalamin injection | 1000 | 200 |
Hydroxocobalamin injection | 1000 | 700 |
Hydroxocobalamin oral | 1000 | 10 |
Hydroxocobalamin oral | 5000 | 50 |
Hydroxocobalamin oral | 15 000 (3 x 5000) | 150 |
Dosage: Initial Therapy
Initial therapy usually involves one (hydroxocobalamin) to two (cyanocobalamin) injections of 1000 µg per week, which corresponds to a daily intake of about 50 to 100 µg per day. This can also be achieved with 5000 – 10 000 µg oral hydroxocobalamin. Initial therapy is continued for about two months.
Dosage: Maintenance Treatment
After successful initial therapy, maintenance doses are administered. Injections are carried out every one or two months, depending on the active ingredient. A daily oral dose of 1000 µg is usual.
Oral Vitamin B12 Therapy
Dosage | Appropriate Supplement | |
Initial therapy | 5000 – 10 000 µg per day | Hydroxocobalamin 5000 µg |
Maintenance treatment | 1000 µg per day | Methylcobalamin, hydroxocobalamin, adenosylcobalamin 1000 µg |
Further reading: Vitamin B12 Dosages and Vitamin B12 Forms
Advantages and Disadvantages: Injection vs Oral Supplements
In the case of severe neurological symptoms, rapid therapy with daily hydroxocobalamin injections is recommended. In many other cases, however, oral supplements can produce equivalent results.
Injections are generally more unpleasant, with a higher risk application. In principle, however, intramuscular injections can also be administered by individuals without a medical background. The advantage of going to a doctor is that the injections are documented and a professional conduct is assured.
The administration of oral supplements is much more pleasant; however it is easy to forget to take them, which can lead to relapses in pernicious anemia. Depending on the dosage, the recovery of blood levels may also take a little longer. One pro of the oral route is that it is much more practical and comfortable, especially if B12 supplements need to be taken for life. Plus, it is also a more natural way of supplying the vitamin.
Vitamin B12, Folic and Iron – A Game of Hide and Seek
The diagnosis of B12 deficiency anemia is still made by GPs on the basis of characteristic blood values: MCV and MCH are significantly elevated; B12 significantly lowered.
Yet unfortunately diagnosis is not always so simple. Firstly, vitamin B12 serum tests can be quite inaccurate and often erroneously delivers high values. Secondly, if there are other nutrient deficiencies at the same time, the blood values can reject this characteristic pattern. Likewise, a B12 deficiency can also mask other deficiencies.
Unreliable: Vitamin B12 Serum Test
The serum test for vitamin B12, which is unfortunately still used today by almost all GPs, has proven to be extremely unreliable (19). This is especially true for pernicious anemia, as this test is extremely distorted by the IF antibodies (20-22). In many cases, a serum test delivers false high values and should therefore not be used to diagnose B12 deficiency.
If B12 anemia is suspected, a combined test should ideally be performed to measure homocysteine and holo TC in the blood, as well as MMA in the urine.
More information: Vitamin B12 Deficiency Test
Synthetic Folic Acid Masks Vitamin B12 Deficiency
When there is a high supply of folic acid and a low B12 level, the blood count appears almost normal. Especially synthetic folic acid supplements can be dangerous in this respect. Blood formation requires a combination of vitamin B12 and folic acid: B12 converts methylfolate back to tetrahydrofolate, which can be used for blood formation. If synthetic folic acid is supplied, tetrahydrofolate is formed in an alternative way – the blood count remains relatively normal despite B12 deficiency. This can be dangerous, as the B12 deficiency will persist and can lead to severe damage to the nerves and spinal cord (23).
Therefore, if possible, L-methylfolate should always be supplemented and B12 deficiency should not be determined by the blood count, but by unambiguous tests such as the holo TC blood test or the MMA urine test.
Iron Deficiency Masks Vitamin B12 Deficiency
In the case of iron deficiency, the haemoglobin content of the red blood cells decreases; the MCH value therefore drops. If vitamin B12 and iron are deficient at the same time, the blood count is ambiguous: MCV is increased, as expected in a B12 deficiency, but MCH is low. This can lead to errors in the interpretation of the blood count, particularly in the case of almost normal or falsely normal B12 values (24-26).
Vitamin B12 Deficiency Masks Iron Deficiency
With a severe B12 and folic acid deficiency, new blood formation can be reduced to such an extent that iron can hardly be utilised. Even with a very poor iron supply, the blood still shows almost normal, sometimes even high, iron levels.
As soon as B12 deficiency is corrected, iron can be utilised once again and iron values drop drastically within a few hours. Only then does the actual iron deficiency become apparent in blood values (27).
When correcting a severe B12 deficiency, it is therefore advisable to also keep an eye on iron levels.
Conclusion: Vitamin B12 Deficiency Anemia
Vitamin B12 deficiency anemia is a dangerous form of anemia, which is today usually recognised and treated in good time. Various interactions can complicate the diagnosis based on the blood count, which is why clear tests such as holo TC or MMA should be used.
In cases of severe anemia, therapy is usually performed with B12 injections, but high-dose oral supplements can also produce equivalent results in cases of impaired absorption. Here doses of at least 5000 µg are required. Hydroxocobalamin is recommended both for injections and for oral use, as this form has particularly good depot properties and can easily be converted into the two active B12 coenzymes.
Sources
- Rojas Hernandez CM, Oo TH (2015) Advances in mechanisms, diagnosis, and treatment of pernicious anemia. Discov Med 19:159–168 PMID: 25828519
- Pruthi RK, Tefferi A (1994) Pernicious anemia revisited. Mayo Clin Proc 69:144–150 PMID: 8309266
- Toh BH, van Driel IR, Gleeson PA (1997) Pernicious anemia. N Engl J Med 337:1441–1448 PMID: 9358143
- Healton EB, Savage DG, Brust JC, Garrett TJ, Lindenbaum J (1991) Neurologic aspects of cobalamin deficiency. Medicine (Baltimore) 70:229–245 PMID: 1648656
- Kumar N (2014) Neurologic aspects of cobalamin (B12) deficiency. Handb Clin Neurol 120:915–926 PMID: 24365360
- Lindenbaum J, Healton EB, Savage DG, Brust JC, Garrett TJ, Podell ER, Marcell PD, Stabler SP, Allen RH (1988) Neuropsychiatric disorders caused by cobalamin deficiency in the absence of anemia or macrocytosis. N Engl J Med 318:1720–1728 PMID: 3374544
- Babio B (1998) Erythrocyte disorders: anemias related to disturbance of DNA synthesis (megaloblastic anemias). Haematol 4th Ed N Y 453–481
- Green R, Datta Mitra A (2017) Megaloblastic anemias: Nutritional and Other Causes. Med Clin North Am 101:297–317 PMID: 28189172
- Toh B-H (2014) Diagnosis and classification of autoimmune gastritis. Autoimmun Rev 13:459–462 PMID: 24424193
- Zittoun J (2001) [Biermer’s disease]. Rev Prat 51:1542–1546 PMID: 11757269
- Lahner E, Annibale B (2009) Pernicious anemia: New insights from a gastroenterological point of view. World J Gastroenterol WJG 15:5121–5128 PMCID: PMC2773890
- Khan S, Del-Duca C, Fenton E, Holding S, Hirst J, Doré PC, Sewell W a. C (2009) Limited value of testing for intrinsic factor antibodies with negative gastric parietal cell antibodies in pernicious anemia. J Clin Pathol 62:439–441 PMID: 19398595
- Annibale B, Lahner E, Fave GD (2011) Diagnosis and management of pernicious anemia. Curr Gastroenterol Rep 13:518–524 PMID: 21947876
- Carmel R (2008) How I treat cobalamin (vitamin B12) deficiency. Blood 112:2214–2221 PMCID: PMC2532799
- Andres E, Serraj K (2012) Optimal management of pernicious anemia. J Blood Med 3:97–103 PMCID: PMC3441227
- Lederle FA (1991) Oral cobalamin for pernicious anemia. Medicine’s best kept secret? JAMA 265:94–95 PMID: 2064638
- Berlin H, Berlin R, Brante G (1968) Oral treatment of pernicious anemia with high doses of vitamin B12 without intrinsic factor. Acta Med Scand 184:247–258 PMID: 5751528
- Andrès E (2014) Oral cobalamin (vitamin B12) therapy in pernicious anemia. Autoimmun Rev 13:778 PMID: 24503031
- Carmel R, Agrawal YP (2012) Failures of Cobalamin Assays in Pernicious anemia. N Engl J Med 367:385–386 DOI: 10.1056/NEJMc1204070
- Vlasveld LT, van’t Wout JW, Meeuwissen P, Castel A (2006) High measured cobalamin (vitamin B12) concentration attributable to an analytical problem in testing serum from a patient with pernicious anemia. Clin Chem 52:157-158; discussion 158-159 PMID: 16391338
- Hamilton MS, Blackmore S, Lee A (2006) Possible cause of false normal B-12 assays. BMJ 333:654–655 PMCID: PMC1570871
- Yang DT, Cook RJ (2012) Spurious Elevations of Vitamin B 12 with Pernicious anemia. N Engl J Med 366:1742–1743 DOI: 10.1056/NEJMc1201655
- Dickinson CJ (1995) Does folic acid harm people with vitamin B12 deficiency? QJM Mon J Assoc Physicians 88:357–364 PMID: 7796091
- Spivak JL (1982) Masked Megaloblastic anemia. Arch Intern Med 142:2111 DOI: 10.1001/archinte.1982.00340250071012
- Carmel R (1988) Pernicious anemia. The expected findings of very low serum cobalamin levels, anemia, and macrocytosis are often lacking. Arch Intern Med 148:1712–1714 PMID: 3401092
- Remacha AF, Sardà MP, Canals C, Queraltò JM, Zapico E, Remacha J, Carrascosa C (2013) Combined cobalamin and iron deficiency anemia: a diagnostic approach using a model based on age and homocysteine assessment. Ann Hematol 92:527–531 PMID: 23183879
- Solmaz S, Özdoğu H, Boğa C (2015) Cobalamin Deficiency Can Mask Depleted Body Iron Reserves. Indian J Hematol Blood Transfus 31:255–258 PMCID: PMC4375157
Photo: Guy Waterval; Apache License 2.0