Vitamin B12 Production by Bacteria
Vitamin B12 is one of the most fascinating and complex biological molecules. While all higher forms of life depend on a supply, vitamin B12 can only be produced by certain bacterial species. Neither plants nor animals have acquired the ability to produce the vitamin themselves in the course of evolution, without the help of bacteria.
As a result, for a long time, all higher organisms were expected to be dependent on an intake of vitamin B12 from food. However, with increasing research into the human microbiome – the collection of bacteria inside and on our body – this understanding has been drawn into question.
It is becoming more and more apparent that complex life forms, such as humans and other animals, may have formed a symbiotic relationship with certain B12-producing bacteria over the course of evolution, which create the vitamin in our intestines and thus contribute to our overall supply. This would be especially good news for vegetarians and vegans who have hardly any B12 sources in their diet.
This article will illuminate this exciting area of vitamin B12 research, which has unfortunately received little attention, and will explore the possibilities and limitations of this type of B12 uptake.
The Human Microbiome
Although the human body consists of between 10-40 trillion cells, this enormous number is far exceeded by the bacterial population that inhabit our body – by almost a hundredfold. With around 100 trillion bacterial cells, bacteria are clearly in the majority (1). Also in regards to genetic material, bacteria surpass us by far: for every human gene in our body there are around 1000 bacterial genes from up to 10 000 different bacterial strains (2).
Our body is therefore far less the autarchic biological machine than modern medicine often considers it to be. Rather, it is a diverse ecosystem in which numerous life forms exist, at best symbiotically, and in which human cells are clearly outnumbered.
Good and Bad Bacteria
While pathogenic bacteria pose a threat to the body, it is now clear that our body’s ecosystem relies on certain benign bacteria to stay healthy. Evolution has led to a symbiosis between humans and these bacterial strains, which are now an integral part of our metabolic system.
Trillions of benign bacteria in our body – as well as constantly changing messenger substances, metabolites, genetic material and nutrients – fulfil extremely important biological tasks. These include: protection against pathogens; assistance in digesting otherwise indigestible proteins, fats and carbohydrates; stimulation of the immune system; and the supply of nutrients (3).
Today, the microbiome is therefore often understood as another vital and highly specialised organ in the human body. What is more, it has also been shown that there is constant communication between the intestinal bacteria and the brain and central nervous system – very similar to that of an ordinary organ (4).
Vitamin B12 Supply through Gut Bacteria
Strains of bacteria found in a healthy human intestine can produce vitamins B1, B2, B5, B6, folate, B12 and K2 and probably also contribute to the supply of these nutrients (5, 6).
In animals, this has been recognised for much longer: ruminants have a special compartment in their stomach, known as the rumen, in which bacteria can produce B12. This is why cows only need a sufficient dietary supply of the trace element cobalt, which bacteria require for B12 synthesis, in order to produce their own supply of the vitamin (7).
The same also applies to fish, for example, which also need cobalt but no dietary B12, as they produce their own supply of the vitamin through symbiosis with bacteria (8, 9). This ability explains why many herbivore species do not require B12 in their diets
It has long been assumed that human intestinal bacteria do not contribute in the same way to the supply of B12, since production of the vitamin takes place mainly in the large intestine, where it can no longer be absorbed. In the 1980s, however, it was shown that B12-producing bacteria also live in the small intestine (10, 11).
Surprisingly, this area has hardly been researched since then and there is a lack of studies on the ideal contribution of intestinal bacteria to the B12 supply. The fact that some long-term vegans, who do not have any B12 sources in their diet, do not suffer from vitamin B12 deficiency suggests that the body’s own supply through gut bacteria might be possible. However, it has not yet been researched as to whether these people might actually be surviving from previously created B12 stores.
Vitamin B12 and Gut Health
The fact that poor intestinal health (and resultant malabsorption) is one of the main causes of vitamin B12 deficiency, suggests that many people are a long way from having a healthy enough gut to enable their body to produce its own supply of B12.
Stress, nutrient deficiencies, antibiotics, drugs and medications – our intestinal flora is today exposed to numerous negative influences. Only as studies into the human microbiome become more popular, do we slowly understand the dramatic impact that poor intestinal health can have on mental and physical health. Comparisons of the microbiomes of indigenous communities that continue to live according to their traditional ways of life, with that of populations in industrialised countries reveal major differences (12).
Vitamin B12 Deficiency and Civilisation Sickness?
In this context, a somewhat old study with Indian migrants in England brought interesting results: while vegetarian Indians in India at that time suffered less frequently from vitamin B12 deficiency, it occurred extremely frequently among Indian migrants living in Britain. Investigations on test participants living in India finally revealed that they possessed certain bacterial strains, through which vitamin B12 production could take place (10).
The research team speculated that through the process of migrating to Britain, as well as the greatly changed hygiene conditions, the ability to self-supply B12 was lost. In later studies, too, the hygienic conditions were blamed for this change in the intestinal flora: the water in India contains considerably more bacteria and the then still customary renunciation of toilet paper led to a greater spread of intestinal bacteria (11).
The loss of large parts of our natural microbiome could therefore also be the result of stringent hygiene. Perhaps this would also explain the increasing prevalence of B12 deficiency in India today.
Poor intestinal health in industrial countries easily develops into a vicious circle: while healthy intestinal flora can resiliently protect itself, a downward spiral develops when intestinal health becomes poor. As intestinal health gets worse, the absorption capacity of nutrients decreases, which in turn has a negative effect on intestinal health. This makes the intestinal flora vulnerable to overgrowth with pathogenic bacteria or fungi, which in turn further destroys the flora and further impairs the uptake of nutrients.
Therefore, not only the gut is important for the B12 supply, but the vitamin is also important for the intestine. A good supply of B12 is vital for the preservation and regeneration of the mucous membranes, which is why the vitamin is critical for regaining intestinal health, and for people experiencing gastrointestinal problems, vitamin B12 supplements are urgently recommended.
Outlook: Vitamin B12 through Probiotics?
However, it is conceivable that in the near future special probiotics – i.e. medicines made from good intestinal bacteria – will be developed which will simultaneously restore intestinal health and the ability to supply bacterial vitamin B12.
But much more research is needed to identify suitable bacterial strains, clinically prove the effectiveness of these therapies and quantify how much B12 these bacteria actually produce and how much the body absorbs.
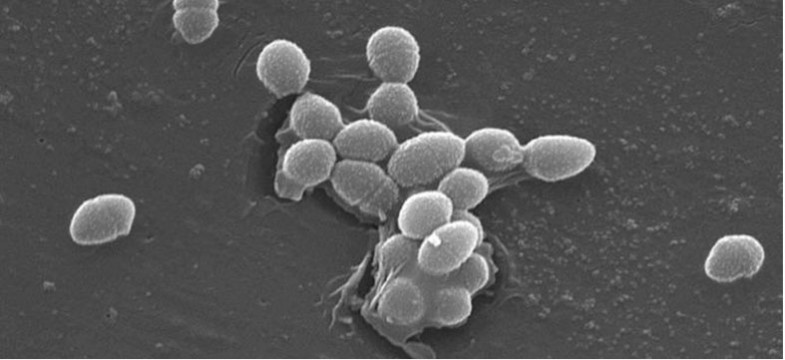
Which Bacteria Produce Vitamin B12?
The first candidates for such a probiotic are already known. However, it remains unclear how to ensure that a sufficient number of the appropriate bacteria inhabit the desired intestinal areas. So far, this has only been achieved through a new therapy method called Faecal Microbiota Transplant (FMT), in which the bacteria are highly concentrated by special intestinal probes in the desired areas of the gut.
However, oral probiotics could also have the desired effect in sufficient dosages – all of these are exciting research fields that will certainly soon gain greater attention.
Here is a list of some known B12-producing bacterial strains – however, some evidence is still missing as to whether or not they all produce real B12 or harmful analogues (13).
Sure
- Propionibacterium freudenreichii (14)
- Propionibacterium shermanii (14)
- Pseudomonas denitrificans (14)
Controversial/unsure
- Lactobacillus reuteri CRL1098 (15-17)
- Pseudomonas sp. (10)
- Klebsiella pneumoniae IIEMP-3 (18)
Vitamin B12, Bacteria and Cobalt
Another area of difficulty is likely to be the cobalt supply. Cobalt is the central atom of B12 and all bacteria need cobalt to synthesise the vitamin.
This is already a major problem in livestock farming: exhausted by intensive agriculture, pasture areas provide less and less trace elements such as cobalt, so that even cattle today are often dependent on B12 or cobalt supplements (19, 20).
The cobalt requirement of humans with an intact intestinal flora has hardly been researched. It is also true that this requirement is mainly covered through vitamin B12. It cannot be ruled out that cobalt supplements and other trace elements may become necessary in the case of a desired B12 supply via intestinal bacteria, since cobalt is hardly found in vegetables anymore. However, this requirement may be covered through some algae.
Conclusion: Vitamin B12 and Gut Bacteria
Research into the human microbiome should herald a paradigm shift in medicine and open up completely new therapeutic options. In terms of nutrient supplies, completely new insights can also be expected in the near future.
Even so, it will be some time before these can be put to practical use. The view that humans are basically not dependent on B12 from food seems somewhat premature against the background of current research: it remains unclear as to what extent which bacteria make a contribution to the supply, whether they can be found in sufficient quantities in the intestines of people in industrialised countries and whether or not the cobalt supply is sufficient.
However, apart from vitamin B12, intestinal health is also an important factor in maintaining general good health and it is to be expected that, in the near future, research into probiotic therapies will gain greater importance. A healthy diet, intestinal treatments and the avoidance of unnecessary antibiotics are already vital building blocks for restoring gut health.
Sources
- Whitman WB, Coleman DC, Wiebe WJ: Prokaryotes: the unseen majority. Proc Natl Acad Sci USA, 1998; 95: 6578–83
- The Human Microbiome Project Consortium: Structure, function and diversity of the healthy human microbiome. Nature, 2012; 486: 207–14
- Guarner F, Malagelada J: Gut flora in health and disease. Lancet, 2003; 361: 512–19
- Mayer EA, Knight R, Mazmanian SK, Cryan JF, Tillisch K. Gut microbes and the brain: paradigm shift in neuroscience. J Neurosci. 2014 Nov 12;34(46):15490-6. doi: 10.1523/JNEUROSCI.3299-14.2014. Review.
- Hill MJ. Intestinal flora and endogenous vitamin synthesis. Eur J Cancer Prev. 1997 Mar;6 Suppl 1:S43-5. Review.
- LeBlanc JG, Milani C, de Giori GS, Sesma F, van Sinderen D, Ventura M. Bacteria as vitamin suppliers to their host: a gut microbiota perspective. Curr Opin Biotechnol. 2013 Apr;24(2):160-8. doi: 10.1016/j.copbio.2012.08.005. Epub 2012 Aug 30. Review.
- Kon, S. K.; Porter, J. W. G. The intestinal synthesis of vitamins in the ruminant. Vitamins and hormones, 1954, 12. Jg., S. 53-68.
- Yu-Hung Lina, Jing-Yun Wua, Shi-Yen Shiau. Dietary cobalt can promote gastrointestinal bacterial production of vitamin B12 in sufficient amounts to supply growth requirements of grouper, Epinephelus malabaricus. Aquaculture Volume 302, Issues 1–2, 1 April 2010, Pages 89–93
- Richard T. Lovell , Tasanee Limsuwan. Intestinal Synthesis and Dietary Nonessentiality of Vitamin B12 for Tilapia nilotica. Transactions of the American Fisheries Society Vol. 111, Iss. 4, 1982
- Albert MJ, Mathan VI, Baker SJ. Vitamin B12 synthesis by human small intestinal bacteria. Nature. 1980 Feb 21;283(5749):781-2
- Baker SJ. Contribution of the microflora of the small intestine to the vitamin b12 nutriture of man. Nutr Rev. 1981 Mar;39(3):147-8.
- Clemente JC, Pehrsson EC, Blaser MJ, Sandhu K, Gao Z, Wang B, Magris M, Hidalgo G, Contreras M, Noya-Alarcón Ó, Lander O, McDonald J, Cox M, Walter J, Oh PL, Ruiz JF, Rodriguez S, Shen N, Song SJ, Metcalf J, Knight R, Dantas G, Dominguez-Bello MG. The microbiome of uncontacted Amerindians. Sci Adv. 2015 Apr 3;1(3).
- J.H. Martens, H. Barg, M.J. Warren, D. Jahn, Microbial production of vitamin B12 , Appl. Microbiol. Biotechnol. 58 (2002) 275–285
- S.A. Survase et al.: Production of Vitamins, Food Technol. Biotechnol. 44 (3) 381–396 (2006)
- Santos F, Vera JL, van der Heijden R, Valdez G, de Vos WM, Sesma F, Hugenholtz J: The complete coenzyme B12 biosynthesis gene cluster of Lactobacillus reuteri CRL1098 . Microbiology 2008, 154 :81-93.
- Taranto MP, Vera JL, Hugenholtz J, de Valdez GF, Sesma F: Lactobacillus reuteri CRL1098 produces cobalamin . J Bacteriol 2003, 185 :5643-5647.
- Santos F, Vera JL, Lamosa P, de Valdez GF, de Vos WM, Santos H, Sesma F, Hugenholtz J. Pseudovitamin B(12) is the corrinoid produced by Lactobacillus reuteri CRL1098 under anaerobic conditions. FEBS Lett. 2007 Oct 16;581(25):4865-70.
- Yulandi A, Sugiokto FG, Febrilina, Suwanto A. Genomic Sequence of Klebsiella pneumoniae IIEMP-3, a Vitamin B12-Producing Strain from Indonesian Tempeh. Genome Announc. 2016 Feb 25;4(1). pii: e01724-15. doi: 10.1128/genomeA.01724-15. PubMed
- Bennets, H. W., et al. Copper and cobalt deficiency of livestock in Western Australia. Journal of Agriculture of Western Australia, 1955, 4. Jg., S. 43-63.
- Suttle, Neville F. Mineral nutrition of livestock. Cabi, 2010